Sinus infection is a common problem that can affect any age group. It represents the fifth most common condition that requires an antibiotic prescription.
Sinuses are four paired air-filled spaces in your skull and face bones surrounding your nose. Their main function is to produce mucus that forms a layer inside the sinuses to humidify inhaled air and keep the interior of your nose moisturized. This mucus layer can trap dust particles, other pollutants, or bad germs and brush them out through your nose. Each sinus drains into your nose through small openings to keep these passages clear of excess mucus and the trapped particles.
However, sometimes, such as when the weather changes and you catch a cold, it can turn into a sinus infection. This causes inflammation of your sinuses, known as sinusitis. Usually, sinusitis should go away in a few days or a week. But sometimes that sinus infection can stick around for a long time.
What is Chronic Sinus Infection?
Chronic sinusitis is a long-standing inflammation of your sinuses that lasts for 12 weeks or longer at a time. Sinusitis is also known as rhinosinusitis (rhino means nose). So, we use the two terms interchangeably. When inflamed, nasal passages and sinuses become swollen and blocked. Chronic sinusitis interferes with the normal drainage of the mucus. Too much mucus builds up in your nose and sinuses, making them stuffy.
What Causes Chronic Sinus Infection?
Multiple factors acting together usually contribute to chronic sinusitis.
People with allergies are more prone to develop chronic sinusitis. About one in five people with chronic sinusitis also have asthma. This is because the linings of your nose and sinuses are in continuation with the linings of your lungs. These people are also likely to have nasal polyps (benign growths in your nose containing mucus).
A bacterial or viral infection can also trigger the condition. The infection is often low grade. The bacteria confine themselves in stubborn “biofilms,” making it difficult for your immune system or antibiotics to find and attack them.
An overlap of additional factors such as smoking, environmental pollutants, and deviated septum, further complicate the picture of chronic sinusitis.
It would be more appropriate to say that if you’re already prone to allergies and nasal polyps, it becomes easier for harmful bugs, especially fungi (molds) to penetrate your sinuses. Likewise, a weak immune system makes you more susceptible to catch bacterial, viral, or fungal sinus infection.
A sinus that is inflamed and swollen can no longer sweep away the excess mucus and harmful agents due to the blockage of tiny hairs that facilitate this function.
What are the Signs and Symptoms of Chronic Sinus Infection?
Chronic sinusitis emerges more insidiously than acute sinusitis. At times, however, the symptoms start suddenly and may resemble that of the common cold or acute sinusitis that just won’t go away.
Chronic sinusitis is most likely if you have two or more of the following symptoms:
- Nasal congestion or stuffy nose
- Mucus and pus-like discharge (yellow fluid draining out of your nose)
- Postnasal drip (mucus dripping at the back of your throat)
- Facial pain, pressure around your eyes and nose, or fullness
- Partial or complete loss of your sense of smell
Chronic cough, sore throat, and fatigue may also be seen in a chronic sinus infection. That said, these symptoms are not required for the diagnosis of chronic rhinosinusitis.
How do you Diagnose Chronic Sinusitis?
The presence of two or more of the listed symptoms for at least three months raises the suspicion of a chronic sinus infection.
In such cases, we will evaluate you to confirm the diagnosis. This involves applying pressure on your sinuses to elicit tenderness. If the tenderness is positive, your sinuses are likely to be inflamed. We will then take a peek into your nose using a small flexible scope, and check for nasal polyps, pus-filled discharge, and deviated septum.
We may also recommend nasal endoscopy. This is an office procedure that enables us to view the interior of your nose and sinus passages. It’s done with an instrument called an endoscope, which is a thin, flexible tube with a tiny camera and a light. We will pass this scope into your nose and sinuses to look inside. Nasal endoscopy allows us to detect any swelling and polyps, as well as collect discharge from the infected area. This can help spot the cause of your infection and what’s the best way to treat it.
If need be, we may also perform imaging in the form of a computed tomography (CT) to look for further problems.
Allergy skin tests look for allergic causes and to check for problems within your immune system may also be done.
What is the Treatment for Chronic Sinus Infection?
When it comes to treating chronic sinusitis, there’s no one-size-fits-all solution. While several treatment options are available, what works for one person may not be appropriate for the other. Hence, we tailor the treatment to each individual’s’ needs, symptoms, and whether or not other conditions (such as allergies or asthma) are also at play.
The goals of treating chronic sinusitis are to address the allergic causes, minimize inflammation, promote free sinus drainage, and eradicate the infection (if there’s any).
Here are a few potential treatment options for chronic sinusitis. We will likely try out a combination of two or more of these options to see what works best for you.
Medical treatment
Saline Nasal Washes
Irrigating your nasal passages with salt water (saline) adds moisture to dry secretions, helps thin the trapped mucus, curbs postnasal drip, and thereby flush out mucus and allergens. It also helps control inflammation.
Glucocorticoid (aka steroid) nasal sprays, washes, and drops
Steroids are highly effective at limiting inflammation. They reduce mucus production and help shrink any polyps. When you use glucocorticoids in the form of nasal sprays or drops, the medicine works right where it is needed.
Nasal steroid sprays do not travel higher up into your sinuses. Instead, they stay and work inside your nose to limit swelling, thus easing sinus drainage into your nasal passages.
If the nasal spray doesn’t work well, we may suggest you adding a nasal steroid solution to the saline nasal wash. This mixture of saline nasal wash and steroid solution pushes the steroid solution higher up into your sinuses to relieve inflammation and ease sinus drainage.
Glucocorticoid pills
Sometimes, we may recommend taking glucocorticoids (steroids) by mouth (orally). These medications, unlike sprays and rinses, reach your circulation and can effectively address inflammation. Despite the dramatic improvement in symptoms with oral steroids, we only prescribe them when it’s necessary. This is because taking steroids by mouth carries some risks, such as suppressing your natural immune system.
Antibiotics
Chronic rhinosinusitis is usually caused by inflammation rather than infection. Bacterial infections may still contribute to sinusitis in some cases. Therefore, some people need to take antibiotics. An adequate antibiotic trial in chronic sinus infection entails a minimum of 3-4 weeks of treatment, preferably culture-guided.
Leukotriene modifiers
We may occasionally prescribe a group of medications called leukotriene modifiers to reduce symptoms of chronic sinusitis. These medications include montelukast (Singulair), zafirlukast (Accolate), and zileuton (Zyflo). They also work by curtailing inflammation but in a different way than steroids.
Immunotherapy shots
If we suspect allergies to be a trigger for your sinusitis, an allergist will also be involved in your treatment strategy. In such cases, we give allergy shots (immunotherapy) that help suppress your body’s immune response to specific allergens (triggers).
Surgical Treatment for Chronic Sinusitis
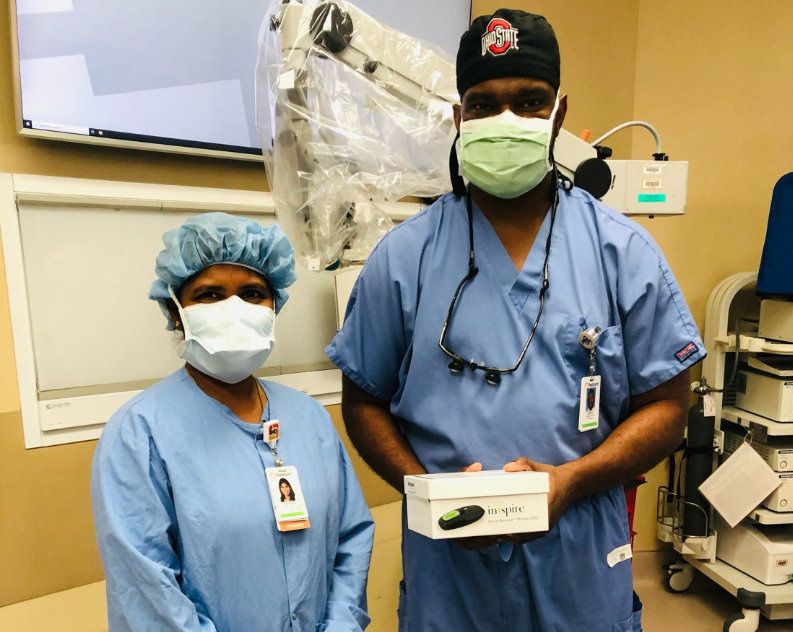
Although medical therapy and lifestyle tweaks are the first-line treatment for chronic rhinosinusitis, some people may fail to respond to optimal therapy. In such cases, Ear, Nose Throat and Allergy Specialist performs a surgery to widen up the blocked sinuses and remove any trapped mucus or polyps.
Other situations in which surgery could be considered include:
- When chronic sinusitis symptoms do not respond to the medical treatments listed above, and CT scan of your sinuses reveals complete blockage of one or more sinuses.
- When nasal polyps fail to shrink enough with steroids.
- When a severe deviation of the septum completely blocks your nose or hinders sinus drainage.
- When there’s a suspicion of allergic fungal sinusitis. The sinuses in allergic fungal sinusitis get clogged with thick, dense mucus that is hard to remove in any way other than surgery.
Balloon Sinuplasty
Our surgeons prefer balloon sinuplasty instead of the traditional endoscopic surgery due to its safety profile, less invasive nature, and faster recovery. However, not all patients are good candidates for balloon sinuplasty. This type of surgery is not a suitable option in patients with nasal polyps or those with severe damage to their sinus openings.
A balloon sinuplasty is an in-office procedure that uses a thin, small, flexible catheter (tube) with an inflatable balloon at its end to reopen blocked sinuses. After passing a balloon catheter, we will slowly inflate it to widen out the sinus opening. We will then wash out all the mucus and pus from your sinus cavity with a saline solution. The balloon is then deflated and removed. This helps reform and widen out the sinuses while maintaining the natural structure of the sinus lining.
It works the same way as balloon angioplasty, in which heart surgeons open up blocked blood vessels.
Most patients can resume their regular activities within a day or two after balloon sinuplasty.
Are you located in the North Georgia area and have a sinus infection that just won’t go away? Contact our office today to schedule an appointment.